Mixing Xanax and Cocaine Can Have Dangerous Results
Written by Megan Hull
& Medically Reviewed by Dr. Conor Sheehy, PharmD, BCPS, CACP
Medically Reviewed
Up to Date
Last Updated - 6/17/2022
View our editorial policy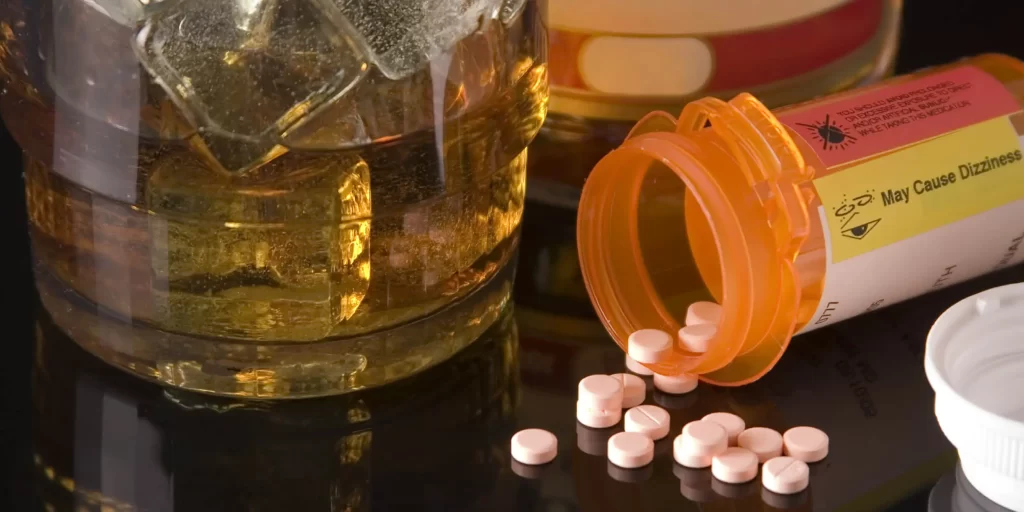
Xanax and alcohol should never be mixed. Xanax is the brand name for the drug alprazolam, a prescription benzodiazepine medication used to treat anxiety and panic disorders. Those prescribed Xanax should have received a warning from their doctor or pharmacist that both it and alcohol are central nervous system (CNS) depressants. Taking these substances together can amplify the effects of both drugs in a dangerous and unpredictable way.
Why Do People Mix Xanax and Alcohol?
People may either mix Xanax and alcohol purposefully or unintentionally. When someone mixes Xanax and alcohol accidentally in low doses, they probably will not experience permanent harm, but they may be more impaired than normal. Xanax can make one drink feel like two or three, and the effects become unpredictable. Many people report temporary memory loss after combining these two substances.
People may also intentionally abuse alcohol and Xanax to heighten the “high.” Abuse of benzodiazepines often occurs in conjunction with other drugs, with about one-fifth of people who abuse alcohol also abuse benzodiazepines.
In the United States, about 408,021 people went to an emergency department for a problem related to benzodiazepine abuse in 2010. About 27.2% of those cases involved both benzodiazepines and alcohol.
Effects of Combining Alcohol and Xanax
Combining Xanax and alcohol increases the CNS depressive effects of each drug. Some symptoms of polysubstance abuse may include:
- Coma
- Dizziness
- Drowsiness
- Impaired motor control
- Increased risk of overdose
- Memory problems
- Slowed or difficulty breathing
- Unusual behavior
Risks of Mixing Xanax and Alcohol
When used at prescribed doses, Xanax can be a safe and effective medication. However, when Xanax is combined with alcohol, the risk of overdose and addiction increases.
During an overdose, people may lose consciousness and stop breathing. In 2010, at least 1,512 people died from mixing benzodiazepines and alcohol.
Since both substances have a high potential for addiction and abuse, using them together is considered polysubstance abuse. During polysubstance abuse, the risk of addiction increases because the crash after using the combination is more intense and uncomfortable. The drive to alleviate the symptoms of the crash by ingesting another substance is what drives addiction.
Overdose on Xanax and Alcohol
If you suspect someone is overdosing, call 911 immediately. Because an overdose is a life-threatening situation, proper medical intervention could save a person’s life.
Symptoms to watch for during an overdose include:
- Altered mental state
- Impaired coordination
- Slowed breathing
- Slowed heartbeat
- Slurred speech
- Stumbling or falling
- Unconsciousness or unresponsiveness
- Vomiting or making gurgling sounds
An overdose of Xanax alone would produce all of the above symptoms, aside from impaired breathing. Benzodiazepines alone do not normally stop breathing during an overdose, which makes their overdoses dangerous but not often fatal. However, when alcohol and Xanax are combined, breathing may slow significantly. Death is much more likely when the two drugs are mixed.
Treatment for Xanax and Alcohol Addiction
Treatment for Xanax and alcohol addiction usually follows the pathway of detox, treatment and maintenance. During detox, the body rids itself of drugs and alcohol. A detox may happen in the rehab facilities, in which case it is termed medical detox because clinicians are on hand to make sure the process is safe.
The next step in treatment is the acute treatment of the addiction and can happen in an inpatient or outpatient setting. During inpatient treatment, clients live in a facility full time and receive around-the-clock medical supervision. Outpatient treatment allows a person to stay living at home.
Finally, after the initial few months, a person enters the maintenance phase. Here, clients continue with sober living and aftercare support as needed.
Rehab facilities like The Recovery Village Ridgefield are experienced in treating polysubstance abuse. While the risk of health harm might be higher for those addicted to more than one substance, help is available. Reach out to a representative today for more information.
Sources
Centers for Disease Control and Prevention. “Alcohol Involvement in Opioid Pain Reliever and Benzodiazepine Drug Abuse–Related Emergency Department Visits and Drug-Related Deaths — United States, 2010.” October 10, 2014. Accessed 24 Aug. 2019.
National Institute on Alcohol Abuse and Alcoholism (NIAAA). “Harmful Interactions.” Accessed Aug 24, 2019.
Schmitz, Allison. “Benzodiazepine Use, Misuse, and Abuse: A Review.” The Mental Health Clinician, May 6, 2016. Accessed Aug 24, 2019.
View Sources
Centers for Disease Control and Prevention. “Alcohol Involvement in Opioid Pain Reliever and Benzodiazepine Drug Abuse–Related Emergency Department Visits and Drug-Related Deaths — United States, 2010.” October 10, 2014. Accessed 24 Aug. 2019.
National Institute on Alcohol Abuse and Alcoholism (NIAAA). “Harmful Interactions.” Accessed Aug 24, 2019.
Schmitz, Allison. “Benzodiazepine Use, Misuse, and Abuse: A Review.” The Mental Health Clinician, May 6, 2016. Accessed Aug 24, 2019.
Authorship






